Introduction
Dose-adjusted R-EPOCH has been widely accepted in the US as the standard frontline chemoimmunotherapy for primary mediastinal B-cell lymphoma (PMBCL) patients (pts) and results in cure without radiation therapy (RT) for the majority of pts. The outcomes of relapsed or refractory (R/R) PMBCL pts have been previously described, but only 7% of these pts received R-EPOCH as initial therapy (Vardhana S, et al. BBMT, 2014). With novel salvage therapy (ST) along with CD19 CAR T-cell therapy (CAR T) now available, evaluating response rates and outcomes to various salvage therapies is paramount to deciding the optimal treatment approach at initial relapse.
Methods
We conducted a multi-center (7 US academic centers) retrospective study of pts with R/R PMBCL. Baseline demographic, clinical, laboratory, pathology, and outcomes data were extracted by chart review. Kaplan Meier was utilized for time to event analysis. Univariate Cox regression analysis was performed for overall survival (OS) and progression-free survival (PFS) with variables described below.
Results
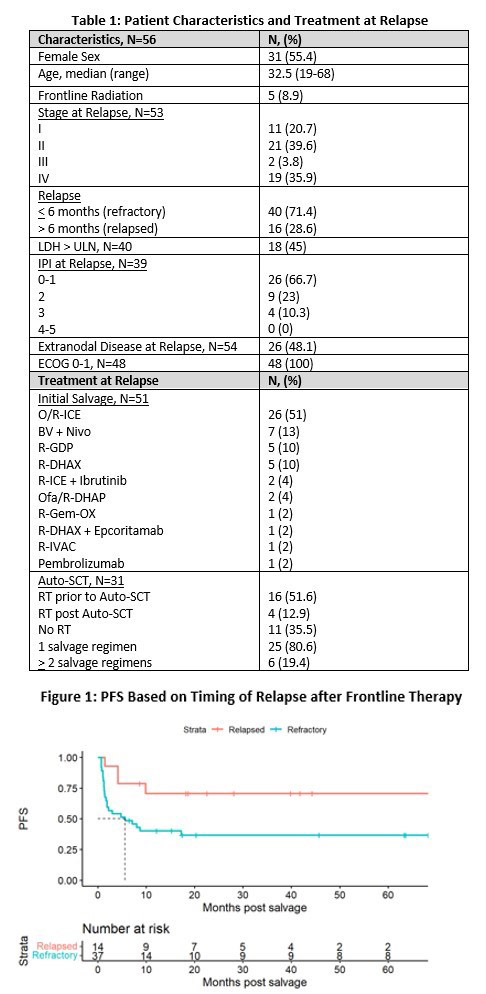
A total of 56 pts who relapsed after R-EPOCH frontline treatment (FT) for PMBCL were identified with characteristics noted in table 1. At relapse, the median age was 32, and the majority were female (55%), with stage I/II disease (60%), LDH < ULN (55%), and refractory to FT (71%). With a median follow up in months of 46.5 (6.2 - 107.1), the 2 yr and 5 yr overall survival (OS) were 92% (95% CI 0.85, 1) and 81% (0.69, 0.94), respectively. There were 9 deaths; 8 attributed to lymphoma and 1 attributed to graft vs host disease after allogeneic stem cell transplant (allo).
Ninety-one percent (51/56) of pts were included in the salvage therapy cohort analysis with exclusions for CNS disease on initial relapse (N=3), receipt of CAR T as 1 st ST (N=1), and no receipt of ST prior to Auto SCT (N=1). ST is detailed in Table 1. The overall response rate (ORR) and complete remission (CR) rate to 1 st line ST for the entire cohort (N=51) was 61% and 31%, respectively. Refractory pts (N=37) and relapsed pts (N=14) had an ORR(CR) rate of 54%(24%) and 78%(50%), respectively, to 1 st line ST. The 2 yr progression-free survival (PFS) for the ST cohort, and refractory, and relapsed subsets was 53% (95% CI 0.41, 0.68), 46% (95% CI 0.32, 0.65), and 71% (95% CI 0.5, 1), respectively. 25% (13/51) received Brentuximab (BV) + Nivolumab (Nivo) salvage therapy as either 1 st line ST (N=7) or 2 nd line ST (N=6) with ORR(CR) rate of 84%(46%) and a 2 yr PFS of 75% (95% CI 53, 100).
Sixty-one percent (31/51) of pts in the ST cohort (19 refractory, 12 relapsed) proceeded to autologous stem cell transplant (ASCT) with a median follow up of 68.5 months. The majority received 1 line of ST prior to ASCT (80%) and RT prior to or post ASCT (65%). Response by PET prior to ASCT was 61% CR, 35% PR, and 3% SD. The 2 yr PFS for all pts receiving ASCT was 83% (95% CI 0.71, 0.98), while the 2 yr PFS for pts in CR prior to ASCT and with SD/PR prior to ASCT was 100% (95% CI 100,100) and 55% (95% CI 0.32, 0.94) respectively.
Variables evaluated in the univariate Cox regression analysis for pts in the ST cohort included LDH at first relapse or progression (> ULN vs < ULN), timing of relapse after FT (rel vs ref), stage at relapse (I vs II-IV), and extranodal disease at relapse (yes vs no). Only LDH > ULN was a predictor of progression after initial ST with HR of 6.72 (1.88,24; p=0.003).
Thirty-four percent (19/56) of pts received CAR T (axi-cel 84%, CAR T on clinical trial 11%, liso-cel 5%), with 1 pt receiving as 1 st line ST and all other receiving as > 2 nd line ST. With median follow up of 39.4 months, the ORR(CR) was 68%(63%), and 2 yr PFS was 68% (95% CI 0.5, 0.93). Thirteen percent (7/56) of pts underwent an allo, and with a median follow up of 40.2 months, had a 2 yr PFS and OS of 0.57 (95% 0.3, 1) and 71% (95% CI 45-100%), respectively.
Discussion
We report the largest cohort of pts with of R/R PMBCL who relapsed after FT R-EPOCH . There was a trend toward worse outcomes in pts refractory to R-EPOCH, but only LDH at relapse > ULN was statistically significant for prediction of progression after 1 st ST. BV+Nivo showed promise as a ST prior to ASCT, but small numbers impede any definitive conclusions compared to traditional salvage options. All 19 pts with CR prior to ASCT remain in remission, highlighting the utility of ASCT in pts achieving a CR to ST. Only 24% of refractory pts had CR to initial salvage. CAR T and allo showed promise as options in pts with multiply relapsed disease.
Disclosures
Sawalha:Beigene: Research Funding; Celgene/BMS: Research Funding; TG Therapeutics: Research Funding. Moskowitz:Bristol-Myers Squibb: Research Funding; Beigene: Research Funding; Incyte: Research Funding; Merck: Honoraria, Research Funding; Seattle Genetics: Honoraria, Research Funding; ADC Therapeutics: Research Funding. Hill:BeiGene: Consultancy; Bristol Myers Squibb: Consultancy; Genentech: Consultancy, Other: Advisory board, Research Funding; Kite, a Gilead Company: Consultancy, Honoraria, Other: travel support, Research Funding; Pharmacyclics: Consultancy, Other: Advisory board, Research Funding; Incyte: Consultancy; Gilead: Other: Advisory board; AstraZeneca: Consultancy; AbbVie: Consultancy, Other: Advisory board, Research Funding. Merryman:Genmab: Membership on an entity's Board of Directors or advisory committees, Research Funding; BMS: Membership on an entity's Board of Directors or advisory committees, Research Funding; Alphasights: Membership on an entity's Board of Directors or advisory committees; Adaptive Biotechnology: Membership on an entity's Board of Directors or advisory committees; Genentech/Roche: Research Funding; Merck: Research Funding; Abbvie: Membership on an entity's Board of Directors or advisory committees; Intellia: Membership on an entity's Board of Directors or advisory committees; Seattle Genetics: Membership on an entity's Board of Directors or advisory committees; Epizyme: Membership on an entity's Board of Directors or advisory committees. Kamdar:Genentech: Other: DMC; syncopation: Consultancy; Genentech: Consultancy; caribou biosciences: Consultancy; Beigene: Consultancy; ADC therapeutics: Consultancy; Adaptive Biotechnologies: Consultancy; Celgene/ Bristol-Myers Squibb: Consultancy; AstraZeneca: Consultancy; SeaGen: Speakers Bureau; AbbVie: Consultancy; Novartis: Research Funding; Celgene: Other: DMC. LaCasce:Research to Practice: Consultancy; Seagen, Kite Pharma: Membership on an entity's Board of Directors or advisory committees. Hess:Bristol Myers Squibb: Consultancy; ADC Therapeutics: Consultancy.